In the gut?
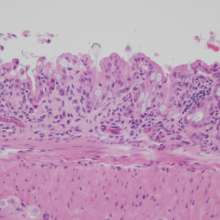
The human gut is home to trillions of microbes, which modulate health and disease.
Our intestinal environment offers a protected, nutrient-rich space for the microbes. The microbes, in turn, give us the benefits of their genes - an evolutionary shortcut such that we do not have to develop new genes for certain capabilities useful for survival. It was estimated that the genes of the microbes living in our gut outnumber our own genes by about 100:1.
The gut microbiota has been shown to carry out functions beneficial to our body such as the digestion of certain food materials, synthesis of vitamins B and K and some amino acids, suppression of harmful pathogenic microbes, detoxification of some potentially harmful substances, and the development of our immune system.
Gut microbiota mediate brain function and behavior changes
Numerous research in the past few years, especially those using germ-free mice, have confirmed the significance of our gut microbiome (microbe's genome) in the development, structure, and functioning of the gut and central nervous systems, as well as the maintenance and integrity of the blood-brain barrier.
Recent research data also show that the balance of the commensal communities of gut bacterial flora plays an important role in the regulation of gut barrier function, the immune system, and the nervous systems. This, in turn, mediate changes in brain function and behavior, such as depression, anxiety, and cognition.
Taken together, a review study published 2016 in the Canadian Journal of Psychiatry suggested that the anxious and depressive symptoms commonly found in post traumatic stress disorder (PTSD) may be associated with changes of the gut microbiota composition and functionality.
Both the composition and the function of the gut bacterial community can be improved through dietary intervention or the use of beneficial bacteria such as probiotics.
Indeed, clinical trials conducted thus far have shown that the administration of different species of Lactobacillus and Bifidobacterium were associated with improvement in mood, reduced anxiety, and decrease in psychological distress, particularly in individuals with low cortisol levels.
This has important therapeutic implications for post traumatic stress disorder (PTSD) patients, who are characterized by long lasting low cortisol levels and dysregulation of the hypothalamus-pituitary-adrenal (HPA) hormonal stress response axis.
The HPA axis has also been shown to be part of the gut-brain axis. An earlier study found that exposing germ-free mice to traumatic stress induced an exaggerated activation of the HPA axis, which was fully reversed by reconstitution with probiotic B.infantis early in life.
Besides low cortisol, PTSD is also marked by increased levels of proinflammatory biomarkers. The review points out that it is interesting to note that cognitive-behavioral therapy (CBT) alone may reduce proinflammatory profile, especially a proinflammatory profile linked to leaky gut.
Another study showed that mice exposed to trauma exhibited decreased gut bacterial diversity and richness associated with increased levels of proinflammatory cytokines in the blood.
Novel therapeutic approaches
Researchers of this review concluded that recent clinical and experimental data converge on the hypothesis that imbalanced gut microbiota, especially in early life, may have long-lasting immune and other physiological effects that make individuals more susceptible to traumatic stress and contribute to PTSD.
The effectiveness of current antidepressant drug therapies in treating PTSD is limited. By considering the gut microbiota as a new biological factor, targeting abnormalities in the disordered systems, and manipulating gut bacterial communities directly through supplementation or indirectly through diet, novel approaches to PTSD treatment may be developed.