Mounting evidence shows that the effectiveness of flu vaccine shots is influenced, and may even be determined, by gut microbes.
The findings of a recent study suggest that gut microbes affect flu shot effectiveness by exerting various effects on immune function, not only by interacting directly with immune cells but also by regulating the availability of metabolites important for immunity.
Background
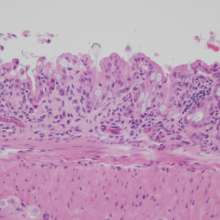
A growing body of evidence suggests that a healthy gut really is the foundation of our health and wellness. Our gut houses over 100 trillion bacteria that have specifically co-evolved with us and form an inner complex and highly diverse ecosystem known as our gut microbiome.
This microbiome plays a key role in the complex mechanisms of immunoregulation. If antibiotics are essential to kill pathogenic bacteria, it is also true that they change the composition and metabolism of the gut microbiome, and the beneficial bacteria that live in human intestines.
About 70% of our immune system resides in and around our gut. The immune system protects against the spread of pathogenic germs in the intestine, but at the same time allows the colonization of beneficial microorganisms. Conversely, the composition of the microorganisms in the intestine influences the quality of any immune reaction.
The majority of the antibiotics available at this moment have a broad spectrum of activity, and they act not only on pathogens but also on beneficial members of the gut microbiota. After antibiotic treatment, gut microbiotas typically take a long time to recover their pre-antibiotic composition.
The study and findings
To study the role of the human gut microbiome in shaping immune responses to seasonal influenza vaccine, a recent study examined the immune responses in antibiotic-treated and non-antibiotic-treated volunteers that received the trivalent inactivated influenza vaccine over two seasons.
Volunteers who received a 5-day course of a broad-spectrum oral antibiotic suffered decreased levels of gut bacteria that were not fully recovered at 6 months, indicating long-lasting loss of unique bacterial species.
Among the participants who had little prior immunity to the seasonal influenza virus vaccine strains, a course of antibiotics hindered their immune responses to H1N1 A/California-specific virus, one of the three influenza virus strains in the vaccine.
As expected, participants who received antibiotics had reduced levels of gut bacteria. Also, the researchers found that, for those with a low immunity to the virus, antibiotic treatment led to fewer antibodies produced in response to the vaccination compared to individuals who had not taken antibiotics.
The antibiotics triggered a pro-inflammatory immune state and altered the metabolic response to the flu vaccination. These findings suggest that those receiving antibiotic treatment prior to vaccination will be less able to mount an immune response when subsequently exposed to this H1N1 virus.
The people who took antibiotics experienced cellular and transcriptional changes within their immune system, which indicates a pro-inflammatory state similar to a condition seen in older adults who have received influenza vaccines.
This pro-inflammatory state was found to be strongly associated with the process by which the microbiome regulates the metabolism of bile acids. A decreased number in the gut flora following antibiotic treatment disrupts bile acid metabolism, which in turn leads to an increase in the inflammatory response.
The findings suggest that gut microbes are able to exert various effects on immune function, not only by directly interacting with immune cells but also by regulating the availability of important metabolites.
Since antibiotics and vaccines are among the most common medical interventions, it is important to understand how the antibiotics affect gut microbiome balance, how the gut microbiota affects immune function and how it could help to boost the efficacy of immunizations.
Our microbiomes play a key role in modulating human immunity. Our microbiomes also change naturally as we age and become less capable of producing immunomodulatory metabolites. These findings and further research could provide insights into why older adults respond differently to influenza vaccination, why they have weaker immune systems overall, and how gut microbiome related interventions may help to boost their immunity and effectiveness of vaccinations for them.