The immune system is often portrayed as our body’s gallant defender, fighting off bacteria, attacking viruses, and protecting us from all those foreign invaders that threaten to make us sick. However, like a chivalrous knight, it is equally important for the immune system to refrain from attacking “friends” and “allies”, such as the body’s own tissues.
When the immune system is no longer able to distinguish between self and non-self, or between harmless and harmful, allergies and autoimmune diseases can result. The immune response can also be a liability in organ transplants, when transplanted tissue is recognized as foreign and destroyed by the immune system.
While scientists have an advanced understanding of the cellular signaling pathways that trigger immune responses, much less is understood about how the body regulates these responses and prevents autoimmunity.
However, recent research suggests that the answer lies in the deeper understanding of the role of dendritic cells, rare immune cells whose branched structure resembles the roots of a tree.
Rare immune cells
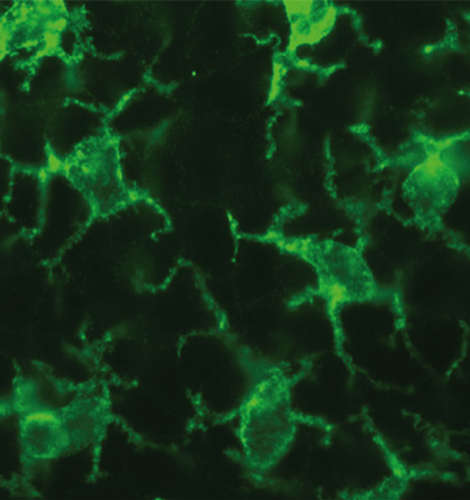
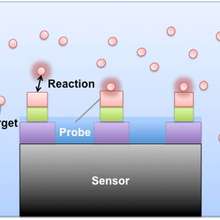
Dendritic cells are found in the skin and mucus tissues of our body where they are exposed to various microbes, viruses, and allergens. Special receptors on their cell membranes allow them to detect potentially harmful foreign bodies and absorb them in a process called endocytosis.
Inside the cell, the pathogens are “chopped up” into smaller pieces called antigens. The dendritic cells then migrate to lymph tissues, where they present these antigens to infection-fighting T and B cells. These antigens stimulate the T and B cells to launch an immune response against the pathogen.
Initiating and directing response
Because of the role dendritic cells play in initiating and directing the immune response, scientists are targeting them in their search for effective treatments against autoimmune diseases and transplant rejection.
In addition to presenting antigens to B and T cells, dendritic cells also release chemical signals that can alter the nature of the immune response. For example, dendritic cells can activate at least three different types of T cells, each of which is most effective at combating a different type of infection.
T H1 cells are most effective at combating bacteria and viruses; TH2 cells are most effective at combating parasitic worms; and, TH17 cells are most effective at combating fungal infections.
Recent research now shows that dendritic cells can also activate a fourth type of T cell called a T regulatory cell or T reg cell. These Treg cells are responsible for regulating the behavior of the other T cells and prevent excess inflammation, allergy, and autoimmunity.
Certain microbes that inhabit the human body, such as Candida Albicans, have evolved mechanisms for decreasing inflammation in the host by programming dendritic cells to activate additional Treg cells.
Scientists are investigating treatments for autoimmunity and transplant rejection, which involve either reducing the number of dendritic cells through drugs such as corticosteroids, or programming dendritic cells to silence immunity by activating additional T reg cells.
Though the latter treatment is still early in development, it has shown promise in studies of diabetes and transplant rejection in mice.