A new gut to lung immune cell recruitment process for rapid immunity is reported in the journal Science.
Background
To protect against a spectrum of pathogens, humans have evolved a large spectrum of immune responses. Innate immune response provides immediate, generic defense, but does not provide long lasting immunity. Adaptive immunity, on the other hand, is acquired and specific to the pathogens.
Allergic mode immune responses are induced by parasite worm helminth infection and a wide range of allergens including peanuts, pollens, venoms, and in rare cases, certain virus and bacteria inflections.
Innate immune lymphoid cells
The new research involved ILC2s, a subtype of a group of immune cells called innate lymphoid cells (ILCs).
These cells are found in low frequency in blood circulation, but rich in mucosal barriers such as intestine and airways, and are considered gatekeepers in mucosal membranes.
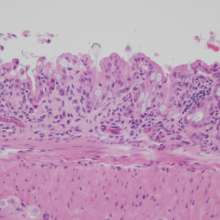
ILCs contribute to immune defense, tissue repair, and metabolic homeostasis in healthy individuals. But they are also involved with the allergic mode of immune responses, and participate in several types of pathologic inflammation including allergy and asthma.
The study
Researchers of this study have previously identified and named a specific population of ILC2s called iILC2s.
In contrast to natural ILC2s, which reside in the lungs during healthy conditions, iILC2s are inflammatory and only arise in the lungs after allergic mode of immune responses were induced.
In the present study, the researchers examine these cells circulating in the blood between two surgically connected, donor and recipient mice. They found that iILC2s were rapidly recruited to the lungs of the recipient mice, and identified the intestine of the donor as the critical origin of these iILC2s.
Further DNA transcriptional analysis showed that iILC2s recruited to the lung are more similar to ILC2s from the small intestine than to the natural lung ILC2s, supporting intestine as the origin.
The recruitment of iILC2s in the lung was transient, and they became undetectable in the recipient mice twelve days into the experiment.
However, further examination of the recipient mice revealed that 10% of natural ILC2s in the lungs and 40% of the ILC2s in the intestine were originated from the intestine of the donor mice, suggesting that iILC2s can return to the intestine, or be converted into natural ILC2s in the lung.
Implications
The researchers suggest that inflammatory iILC2s and natural ILCs serve distinct and important purposes in the lung:
- Inflammatory iILC2s are recruited from the intestine for rapid and transient immune responses
- Natural ILC2s are mainly lung tissue-resident and can potentially give rise to memory ILC2s for faster and more efficient response when the immune challenge is repeated.
They conclude that innate immune ILCs cells complement adaptive immunity, providing both local and distant tissue immune responses during infection.
A potential clinical implication from the study is that therapies targeting disturbance in gut microbiota may also interfere with the ILC gut-lung axis, thereby reducing pathogenic inflammation in allergies and asthma.