Scientists reported that antibiotic resistance in common pathogens increases with regional temperature and population density across the US.
The associations between temperature and antibiotic resistance are consistent across most classes of antibiotics and pathogens, and their resistance may be strengthening over time.
Background
Since the discovery of penicillin in 1928, antibiotics have dramatically reduced bacterial infections and the associated morbidity and mortality. Penicillin has increased the survival rate from 10% to 90% for patients with pneumonia and blood infection.
However, bacteria that cause infections in human can develop or acquire resistance to antibiotics commonly used against them. Antibiotic resistance causes significant morbidity worldwide.
According to the World Health Organization (WHO), deaths attributed to antibiotic resistance could reach 10 million a year by 2050, costing the world up to US$100 trillion. By comparison, the WHO estimated deaths attributed to cancer could reach 8.2 million a year by 2050.
Antibiotic resistance is largely due to selective pressure of antibiotic use. Global use and overuse of antibiotics have contributed to the spread of antibiotic resistance.
In this study, the American and Canadian researchers examined factors other than selective pressure that may contribute to the increase of antibiotic resistance.
The study
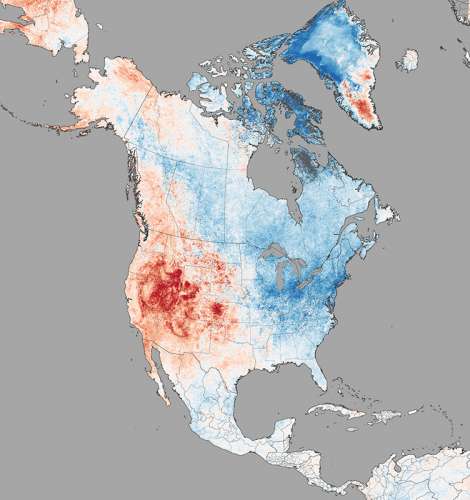
The study investigates and analyses whether regional characteristics such as local temperature, population density, antibiotic prescription rate, and other factors could explain the differences in antibiotic resistance across different regions in the US.
The researchers focus on 3 most commonly reported resistant bacteria, which are common community- and hospital-acquired bacterial pathogens. They are:
- E. coli (causes severe diarrhea, genital and urinary tract infections)
- K. pneumoniae (major cause of healthcare-associated infections including pneumonia, blood and wound infections, and meningitis)
- S. aureus (common cause of serious infections including sepsis, pneumonia, heart valves and bone infections)
Using information sourced from 223 facilities across 41 US states including hospitals, laboratories, and infection surveillance units, the researchers generated 602 indices for the years 2013-2015 and developed a large database of antibiotic resistance patterns.
They then examined the relationships between the regional patterns of antibiotic resistance and historical regional temperatures during the time when the antibiotic patterns developed.
Findings
The results showed that an increase of 10o C across regions was associated with an increase in resistance to antibiotics of 4.2% for E. coli, 2.2% for K. pneumoniae, and 2.7% for S. aureus, after adjusting for prescription rate, population density, acquisition source, and laboratory standard.
Increasing antibiotic resistance with increasing temperature is consistent across most classes of antibiotics and pathogens.
The researchers also examined S. aureus resistance to specific antibiotics, and found that with a 10o C increase across regions, its resistance to cloxacillin increased by 5.8%, fluoroquinolones by 3.7%, and macrolides by 6%.
The results also showed that an increase in population density by 25,900 persons per square kilometer (10,000 persons per square mile) was associated with 6% increase in antibiotic resistance for K. pneumoniae, and 3% for E. coli.
Implications
Researchers suggested that temperature is one of the strongest modifiers of bacteria growth rates. Higher temperature may drive increased carriage and transmission of resistant strains of pathogens between humans, and animals. It may also facilitate the transfer of resistant pathogen genes.
They cautioned that in the face of global population growth and climate change, the impact and burden of antibiotic resistance might have been significantly underestimated. Further research to confirm their findings is needed. This study is published in the journal Nature Climate Change.