It is clear that intense, massive, terrifying, and/or chronic traumatic experiences can result in the development of post traumatic stress disorder (PTSD), and, those with PTSD carry a higher risk of developing other mental health problems such as anxiety, depression, alcohol/drug abuse, and suicide thoughts/attempts.
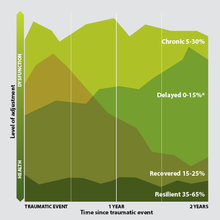
However, not all who were exposed to traumatic experiences develop PTSD as a result. The factors underlying susceptibility and resilience to traumatic stress are still not clear, but biological markers and factors predisposing an individual to these traits are beginning to emerge.
Inflammatory immune response
In a 2014 prospective clinical study of more than 1,800 war-zone deployed marines and navy combatants, it was found that their proinflammatory C-reactive protein (CRP) levels measured before deployment were significantly associated with PTSD post deployment.
Researchers suggest that CRP levels may be linked with susceptibility or resilience for PTSD.
Even though correlations do not imply a cause-effect relationship, numerous studies have found positive correlations between depression and the levels of proinflammatory cytokines, especially interleukin (IL)-6, tumor necrosis factor-α, and C-reactive protein.
Recent experimental and clinical studies have highlighted the predictive value of proinflammatory biomarkers in the development of psychological symptoms.
A 2014 study showed that compared to resilient mice, susceptible mice had increased leucocyte count (immune cells), which released higher amounts of IL-6 in response to acute stress.
Results suggest that dysregulated immune physiology and higher proinflammatory cytokines are risk factors for stress susceptibility.
Previous traumatic experience
Epidemiological studies show that traumatic stress in childhood can influence the onset of psychiatric conditions such as depression and anxiety later in life. It is estimated that up to 82% of children will experience at least one traumatic experience before adulthood.
In particular, childhood maltreatment including physical abuse, sexual abuse and neglect is a consistent predictor of PTSD, with maltreated children 5 - 10 times more likely to develop clinical PTSD as a young adult than those not maltreated. It is estimated that maltreatment affects 700,000 children under the age of 18 each year in the US.
The prevalence of PTSD is estimated to range between 30-37% in adults with documented history of childhood maltreatment, much higher than around 7% found in the general population. Childhood maltreatment poses an increased risk both for childhood PTSD and PTSD throughout the lifespan.
The underlying mechanisms are still not clear. But studies have shown that early traumatic stress lead to a proinflammatory phenotype, and alteration of hippocampal neurogenesis that could have long lasting negative effects.
A meta-analysis study in 2015 confirmed that childhood trauma contributes to a proinflammatory state in adulthood. This, in turn, predicts and predisposes individuals to develop PTSD after a traumatic event later in life.
Dysregulation of cortisol stress response
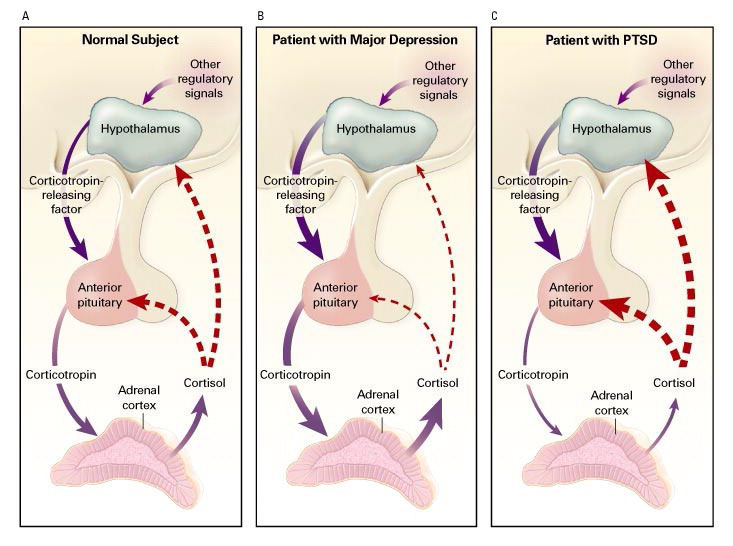
Depression is associated with increased levels of proinflammatory biomarkers and abnormal responses to stress. PTSD seems to be marked in addition by low cortisol levels.
The hypothalamus, the pituitary gland, the adrenal hormonal gland, together with their interactions constitute the hypothalamic-pituitary-adrenal axis (HPA axis).
It is a major neuroendocrine system that controls stress response and regulates many body processes including digestion, immune response, mood and emotions, sexuality, and energy storage and expenditure.
Stimulation of this axis results in increased hypothalamic secretion of corticotropin-releasing hormone (CRH). CRH then stimulates the pituitary to produce adrenocorticotropin (ACTH). Blood levels of these hormones can increase two- to fivefold during traumatic stress in humans.
When ACTH is transported to the adrenal gland, it rapidly stimulates the biosynthesis of corticosteroids such as cortisol, a major stress hormone. Cortisol affects many physiological functions of the body and the brain.
In an important negative feedback loop, cortisol inhibit both the hypothalamus and the pituitary gland, reducing the secretion of CRH and ACTH to down regulate traumatic stress responses.
PTSD is thought to be reflecting sustained, chronic stress reactions to a traumatic experience. However, although PTSD patients have high levels of CRH, they consistently have unexpectedly low levels of cortisol compared with healthy individuals.
This suggests dysfunctional negative feedback loops in the HPA axis, which failed to contain stress responses.
Disruption of the HPA axis appears to be sustained as low cortisol levels persist, even decades after the initiating traumatic experience.
In fact, research evidence showed that low cortisol concentration in the blood immediately after a trauma predicts subsequent PTSD diagnosis.
Emerging research findings also show that low cortisol levels shortly after a traumatic event reflects previous traumatic experience and predisposes PTSD later in life.
Brain biomarkers
Research suggest that the effects of chronic stress are associated with changes in the expression of genes involved in certain neurotrophic activity and neurotransmission. Some brain biomarkers are associated with susceptibility or resilience to chronic stress.
Brain-derived neurotrophic factors (BDNF) are molecules that support the growth, survival and differentiation of neurons. Studies show that increased levels of BDNF (a key regulator of the dopamine reward pathway) and signalling in the nucleus accumbens (significant players in addition, cognitive processing of motivation, reward, positive reinforcement, learning, processing fear, and impulsivity) induced susceptibility to stress in mice.
Postmortem brain analysis of depressed patients also revealed that the protein expression of BDNF was increased in the nucleus accumbens compared to non-depressed individuals.
Another 2014 study showed the potential role of γ-aminobutyric acid (GABA) receptors in influencing avoidance and depression-like behavior in mice. Mice lacking GABA-B(1a) receptors were susceptible whereas those lacking GABA-B(1b) receptors were resilient to chronic stress-induced abnormalities.
Taken together, it is increasingly evident that advancing research is helping to identify those at greatest risk for PTSD on the basis of biological, not only psychological, characteristics.
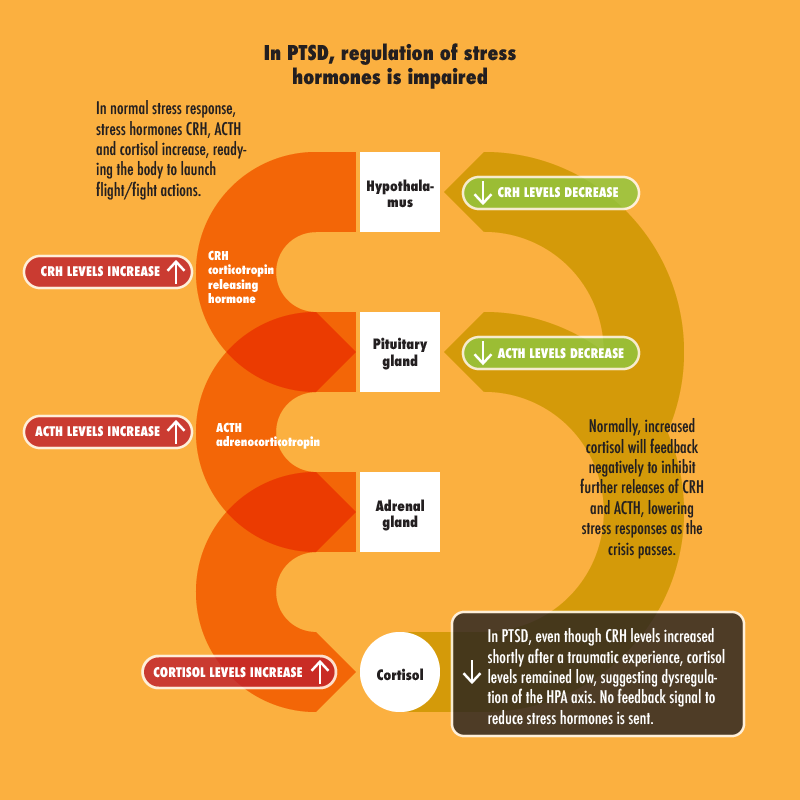
CRH corticotropin releasing hormone, ACTH adrenocorticotropin, Cortisol
CRH, ACTH and cortisol hormones increased in response to stress/trauma, readying the body to launch flight/fight actions.
Normally, increased cortisol will feedback negatively to inhibit further releases of CRH and ACTH, down regulating stress responses as the crisis passes.
In PTSD, even though CRH levels increased shortly after a traumatic experience, cortisol levels remained low, suggesting dysregulation of the HPA axis.